Who should be screened for *possible* ADHD?
If you see patients with mental health problems—especially depressive disorders, anxiety disorders, and substance use disorders— you can be sure that you are missing the underlying or additional diagnosis of ADHD in at least some of them. Don’t believe me? Try the screening method explained on this page with every single one of your patients for one week, then send me an email at mago@simpleandpractical.com to tell me how wrong I was. 🙂
It is not practical to do a full ADHD evaluation on every patient we see. The word “screening” refers to briefly evaluating patients who are not known to have the disorder and are not even specifically suspected of having the disorder.
Bottom line: I recommend that all patients we see—especially those with mood or anxiety disorders and substance use disorders—should be screened for a possible primary or additional diagnosis of ADHD.
Note: An important practice guideline recommended that family members of patients with ADHD should also be screened (Kooij et al., 2019).
Extremely important!
Every patient with “treatment-resistant depression” MUST be very carefully evaluated for a missed diagnosis of bipolar disorder and/or ADHD. It is by doing this that I first realized that many of the patients who had been referred to me due to their depression not responding to numerous medications had either bipolar disorder or a comorbid diagnosis of ADHD, which was a big reason for the patients being depressed.
Who does not need to be screened for ADHD?
Note: If a patient comes in specifically for suspected ADHD, the evaluation would not be called screening. Those patients don’t require screening because they are already suspected of possibly having ADHD. In such cases, ADHD would be the main focus of the psychiatric evaluation.
Use the Adult ADHD Self-Report Scale (ASRS)
The most commonly used way to screen adult patients for a possible diagnosis of ADHD is to have every patient fill out the Adult ADHD Self-Report Scale (ASRS; Kessler et al., 2005). The scale is in the public domain and is available for download and use at no cost at any of the links below. Several links are provided in case one of them stops working in the future.
https://www.adhdawarenessmonth.org/wp-content/uploads/psych_adhd_checklist.pdf
https://add.org/wp-content/uploads/2015/03/adhd-questionnaire-ASRS111.pdf
https://www.hcp.med.harvard.edu/ncs/asrs.php
Alternatively, the ASRS can also be completed online at the following link:
https://tests.add.org/
The scale consists of 18 items that correspond to the DSM-5-TR® diagnostic criteria for ADHD. This 18-item Adult ADHD Self-Report Scale (ASRS) is also referred to as the ASRS Symptom Checklist.
The first 6 items of the ASRS have greater value for screening even though the scale has 18 items (Kessler et al., 2007). These 6 items are also called the ASRS Screener, which can be sufficient for screening if you would rather keep it as brief as possible. But I just have my patients complete the full 18-item version because the other items provide additional information, and I would rather err on the side of identifying a patient as having possible ADHD and do an evaluation rather than make a mistake in the other direction.
How to score and interpret the ASRS
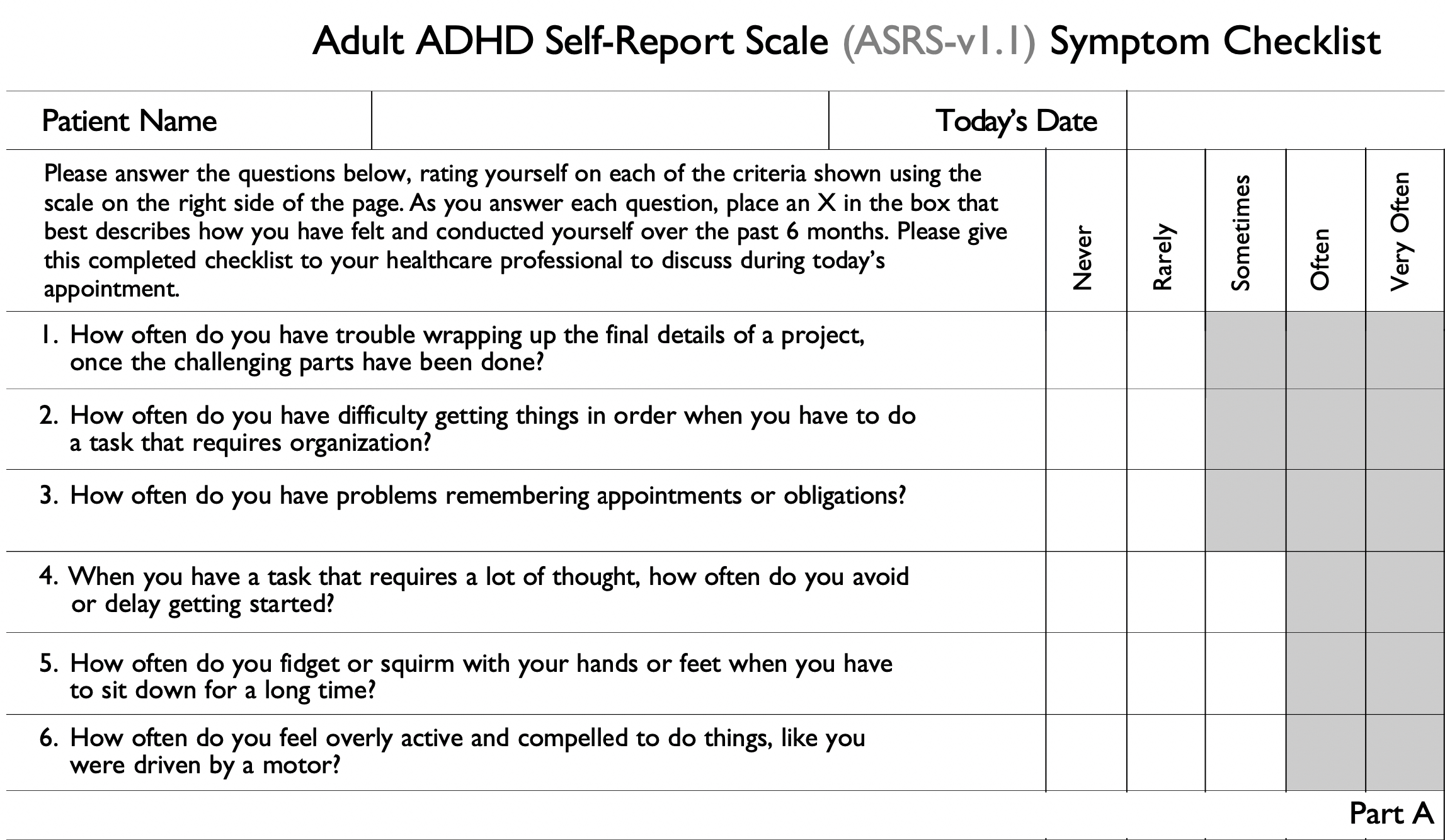
– The image above shows the first 6 questions of the Adult ADHD Self-Report Scale (ASRS), which are called “Part A”. An “abnormal” rating on any of the items is indicated on the scale by the fact that those boxes have a grey background.
– Obviously, we should not tell patients that a checkmark in a grey area counts towards the possibility of ADHD because it could bias the responses of some patients. (By the way, if you wanted to remove the grey background to avoid biasing patients, though I’m not sure that this is needed, one way to do this is to print out the document and photocopy it using a light sighting on the photocopy machine.)
– If a patient scores 4 or more out of the first 6 items in the abnormal range, this suggests that the person may have ADHD, and a full clinical evaluation is indicated.
– What about the remaining 12 questions of the ASRS (“Part B)”? They provide additional information and alert us to problems that we should ask the patient about. Various total scores using all 18 questions have been evaluated in research studies, but it is recommended that only the first 6 questions of the ASRS be used to indicate that the person may have ADHD.
EXTREMELY important tip for reducing false positives on the ASRS
In my opinion, it is crucial, when using the Adult ASRS scale to screen a patient presenting with depression, anxiety, etc, to ask the patient to answer the questions for their “lifetime,” that is, “before the depression (or anxiety).”
This is because when patients are significantly depressed or anxious, of course, they will have some symptoms similar to those of ADHD. On the other hand, ADHD symptoms, by their very nature, have been present since relatively early in life.
In my clinical experience, doing what I recommended above is EXTREMELY important! By doing this, I have tremendously reduced my “false positive” rate. I don’t end up wasting a lot of time evaluating patients in detail for ADHD only to realize that they were describing symptoms that they had only since they became clinically depressed or anxious.
Other tips on using the ASRS
1. Even if the patient screens negative, it does not definitely rule out ADHD. If we get a history in childhood or adulthood that could be suggestive of ADHD, we should go ahead and ask about the symptoms of ADHD, even if the ASRS score did not suggest possible ADHD.
2. My personal recommendation is that if any items are scored in the abnormal range (grey areas), we should ask more about that symptom to try to understand why the patient has that problem.
Related Pages
ADHD—Screening
How to screen all your patients for Adult ADHD
Why don’t we screen every patient for adult ADHD?
ADHD—Evaluation
Tips on history-taking in evaluating adults for possible ADHD
Neuropsychological testing for diagnosing ADHD?
What is the role of neuropsychological testing in patients with ADHD?
What neuropsychological deficits may be present in patients with ADHD?
ADHD—Treatment—General
Tips for prescribing ADHD medications
Converting stimulants: Equivalent doses
A dozen tips to manage loss of appetite due to a stimulant (in adults)
Tips for managing abuse potential of medications for ADHD
Does lisdexamfetamine really have lower abuse potential?
How are methylphenidate and amphetamines metabolized?
Combine a stimulant and atomoxetine?
Pros and cons of short-acting preparations of psychostimulants
Converting from OROS methylphenidate to amphetamine is a two-step process
Stimulant medications and irritability in children with ADHD
What if you refuse an early refill of a stimulant medication?
What to look for in stimulant withdrawal (including a physical sign that is little known)
Stimulant “holidays” (breaks) in adults with ADHD?
How to get full-day coverage with stimulants
Eight tips for reducing the risk of abuse/diversion of stimulants
Can psychostimulant medications cause or worsen Raynaud’s phenomenon?
Laws about prescriptions for psychostimulants
Are stimulants useful after traumatic brain injury?
ADHD—Treatment—Methylphenidate preparations
Methylphenidate preparations: Index and links
Should we prescribe dexmethylphenidate (Focalin) rather than methylphenidate (Ritalin)?
Converting from OROS methylphenidate to amphetamine is a two-step process
Should we combine methylphenidate and guanfacine?
Methylphenidate (Ritalin, Ritalin SR®, Ritalin LA®): Basic information
Dexmethylphenidate (Focalin®, Focalin XR®): Basic Information
First ADHD medication to be taken at *bedtime*–Why? How?
ADHD—Treatment—Amphetamine preparations
Amphetamine preparations: Index and links
Pros and cons of dextroamphetamine versus levoamphetamine
Does lisdexamfetamine really have lower abuse potential?
Amphetamine (Dynavel-XR®) extended-release oral suspension: Basic information
Amphetamine extended-release orally disintegrating tablets (Adzenys XR-ODT): Basic information
What is the maximum dose of mixed amphetamine salts?
Dextroamphetamine (Dexedrine®): Basic Information
Lisdexamfetamine (Vyvanse®): Basic Information
Mixed amphetamine salts (Adderall®, Adderall XR®): Basic Information
Mixed salts of a single-entity amphetamine product (Mydayis®): Basic information
Triple-bead preparation of mixed amphetamine salts (Mydayis®)
Ketogenic diet and amphetamines
ADHD—Treatment—Atomoxetine
Atomoxetine (Strattera®): Basic Information
Don’t ignore atomoxetine for ADHD in adults
Order genetic testing for a patient on atomoxetine?
Seizure risk if atomoxetine and bupropion are used together?
Combine a stimulant and atomoxetine?
It makes a big difference—atomoxetine once a day or twice a day?
What can we do for somnolence/ sedation on atomoxetine?
ADHD—Treatment—Alpha-2 agonists
Clonidine (Kapvay®) extended-release tablets: Basic Information
Guanfacine versus clonidine for ADHD
Guanfacine (Intuniv®): Basic Information
Should we combine methylphenidate and guanfacine?
Guanfacine versus clonidine for ADHD
Does guanfacine work for ADHD in adults?
ADHD—Treatment—Other medications
Do you prescribe bupropion for ADHD in adults?
Does modafinil work for ADHD?
Viloxazine extended-release (Qelbree®): Basic information
ADHD—Treatment—Psychotherapy
Tips for remembering to do things
Drug interactions involving ADHD medications
Important interactions when using two medications for ADHD
Vitamin C if on a stimulant?
Seizure risk if atomoxetine and bupropion are used together?
Be careful if a person is on both a stimulant and an antipsychotic
What could happen when changing from an antipsychotic to a stimulant?
Can a dopamine agonist (pramipexole, ropinirole) and a stimulant be combined?
Ketogenic diet and amphetamines
ADHD with comorbid disorders
Comorbid Bipolar Disorder and ADHD
How common is ADHD in persons with bipolar disorder?
How to treat ADHD in persons with bipolar disorder
Stimulants for ADHD with a history of a substance use disorder?
How should ADHD be treated in persons with stimulant (including cocaine) use disorder
ADHD—Resources
BEST Books on Adult ADHD: for Clinicians
BEST Books on Adult ADHD: For Patients and/or Families
Book Review: ADD-Friendly Ways to Organize Your Life
Book review: Mindfulness Prescription for ADHD
Alarmy: An alarm that makes you PROVE that you are really awake!
ADHD as a difference in cognition, not a disorder. Talk from TEDx (YouTube video)
Four C’s for dealing with ADHD (YouTube video)
Things that can masquerade as ADHD (YouTube video)
ADHD—Miscellaneous
Childhood ADHD: Persistence into adulthood
For links to all the articles on this website that are related to ADHD and its treatment, please see:
Attention-Deficit/ Hyperactivity Disorder (ADHD): Main Menu
References
Adler LA, Faraone SV, Sarocco P, Atkins N, Khachatryan A. Establishing US norms for the Adult ADHD Self-Report Scale (ASRS-v1.1) and characterising symptom burden among adults with self-reported ADHD. Int J Clin Pract. 2019 Jan;73(1):e13260. doi: 10.1111/ijcp.13260. Epub 2018 Sep 21. PMID: 30239073; PMCID: PMC6585602.
Anbarasan D, Kitchin M, Adler LA. Screening for Adult ADHD. Curr Psychiatry Rep. 2020 Oct 23;22(12):72. doi: 10.1007/s11920-020-01194-9. PMID: 33095375.
Ginsberg Y, Quintero J, Anand E, Casillas M, Upadhyaya HP. Underdiagnosis of attention-deficit/hyperactivity disorder in adult patients: a review of the literature. Prim Care Companion CNS Disord. 2014;16(3):PCC.13r01600. doi: 10.4088/PCC.13r01600. Epub 2014 Jun 12. PMID: 25317367; PMCID: PMC4195639.
Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, Ustun TB, Walters EE. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005 Feb;35(2):245-56. doi: 10.1017/s0033291704002892. PMID: 15841682.
Kessler RC, Adler LA, Gruber MJ, Sarawate CA, Spencer T, Van Brunt DL. Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) Screener in a representative sample of health plan members. Int J Methods Psychiatr Res. 2007;16(2):52-65. doi: 10.1002/mpr.208. PMID: 17623385; PMCID: PMC2044504.
Kooij JJS, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, Thome J, Dom G, Kasper S, Nunes Filipe C, Stes S, Mohr P, Leppämäki S, Casas M, Bobes J, Mccarthy JM, Richarte V, Kjems Philipsen A, Pehlivanidis A, Niemela A, Styr B, Semerci B, Bolea-Alamanac B, Edvinsson D, Baeyens D, Wynchank D, Sobanski E, Philipsen A, McNicholas F, Caci H, Mihailescu I, Manor I, Dobrescu I, Saito T, Krause J, Fayyad J, Ramos-Quiroga JA, Foeken K, Rad F, Adamou M, Ohlmeier M, Fitzgerald M, Gill M, Lensing M, Motavalli Mukaddes N, Brudkiewicz P, Gustafsson P, Tani P, Oswald P, Carpentier PJ, De Rossi P, Delorme R, Markovska Simoska S, Pallanti S, Young S, Bejerot S, Lehtonen T, Kustow J, Müller-Sedgwick U, Hirvikoski T, Pironti V, Ginsberg Y, Félegyházy Z, Garcia-Portilla MP, Asherson P. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur Psychiatry. 2019 Feb;56:14-34. doi: 10.1016/j.eurpsy.2018.11.001. Epub 2018 Nov 16. PMID: 30453134.
Ustun B, Adler LA, Rudin C, Faraone SV, Spencer TJ, Berglund P, Gruber MJ, Kessler RC. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry. 2017 May 1;74(5):520-527. doi: 10.1001/jamapsychiatry.2017.0298. Erratum in: JAMA Psychiatry. 2017 Dec 1;74(12):1279. Erratum in: JAMA Psychiatry. 2019 Nov 1;76(11):1213. PMID: 28384801; PMCID: PMC5470397.
van de Glind G, van den Brink W, Koeter MW, Carpentier PJ, van Emmerik-van Oortmerssen K, Kaye S, Skutle A, Bu ET, Franck J, Konstenius M, Moggi F, Dom G, Verspreet S, Demetrovics Z, Kapitány-Fövény M, Fatséas M, Auriacombe M, Schillinger A, Seitz A, Johnson B, Faraone SV, Ramos-Quiroga JA, Casas M, Allsop S, Carruthers S, Barta C, Schoevers RA; IASP Research Group; Levin FR. Validity of the Adult ADHD Self-Report Scale (ASRS) as a screener for adult ADHD in treatment seeking substance use disorder patients. Drug Alcohol Depend. 2013 Oct 1;132(3):587-96. doi: 10.1016/j.drugalcdep.2013.04.010. Epub 2013 May 6. PMID: 23660242; PMCID: PMC4083506.
Copyright © 2016 to 2026, Simple and Practical Medical Education, LLC. All rights reserved. The content on this website may not be reproduced in any form without express written permission.
Disclaimer: The content on this website is provided as general education for medical professionals. It is not intended or recommended for patients or other laypersons or as a substitute for medical advice, diagnosis, or treatment. Patients must always consult a qualified healthcare professional regarding their diagnosis and treatment. Healthcare professionals should always check this website for the most recently updated information.
Dr. Mago, first off, thank you for a truly comprehensive yet eminently pertinent and truly simple but practical information.
About the ASRS, why does it ask about the past 6 months? I tell my patients that they should try to recall as far back as they can. I also tell them, if they are taking ADHD medications, to try and recall how things were BEFORE they started the medication. I often ask a spouse or partner to fill out the ASRS with their observation of the patient as well and then interview them too.
Thanks again for your truly remarkable support and educating of fellow psychiatrists.
Mo Dattu, MD
Doesn’t ADHD screeners have a low change of providing an accurate diagnosis since the false positive rates are so high?
https://pubmed.ncbi.nlm.nih.gov/37366274/
Your question has now been answered in the following article on this website: Screening questionnaires SCREEN, not DIAGNOSE
This was really helpful. I think that we should screen every patient at least IMO. I can’t stop thinking that some of my patients with depression or anxiety don’t get better on the cognitive side because they have a comorbidity like ADHD
Thanks, Dr. Villalobos. I 100% agree with you!
This may have been answered elsewhere but is there a threshold number of questions in part B to suggest a problem?