By Rajnish Mago, MD (bio)
On another page on this website, I emphasized the reasons why we should routinely use self-rated scales to screen for OCD, evaluate patients with OCD, and monitor the progress of treatment.
The scale that Simple and Practical Medical Education recommends for screening patients for possible OCD is the Obsessive-Compulsive Inventory-Revised (OCI-R; Foa et al., 2002; Huppert et al., 2007). It has specifically been shown to be good for this purpose (Foa et al., 2002).
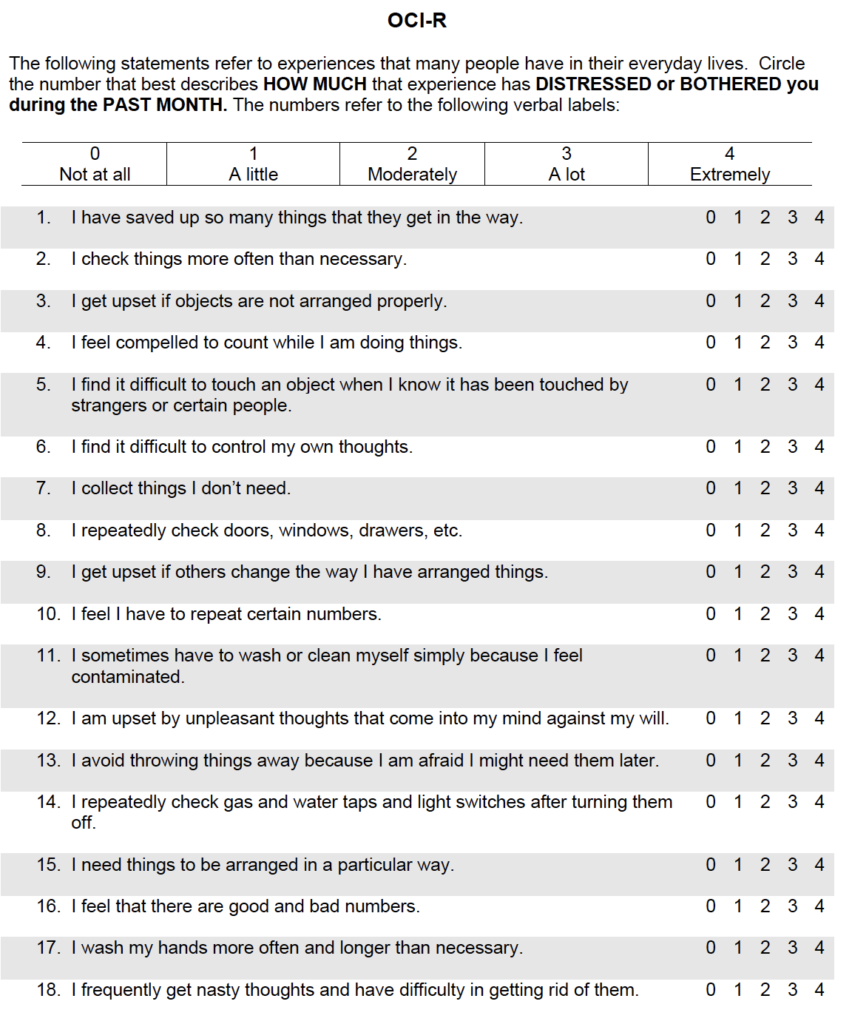
Obsessive-Compulsive Inventory-Revised (OCI-R)
The OCI-R (Foa et al., 2002; Huppert et al., 2007) is in the public domain, which means that anyone can use it free of cost and without getting permission from the authors. It can be downloaded for use in your clinical practice by clicking on the link below:
OCI-R
Symptoms and their categories
Take a look at the questions on the OCI-R below.
This inventory has 18 items. It evaluates six groups of OCD symptoms with three items for each group. The groups of symptoms are: washing, checking, ordering, obsessing, hoarding, and neutralizing. Since the questions are mixed up, these groups are not immediately obvious in looking at the questions. Can you look at the 18 items and figure out which ones are related to washing, checking, ordering, obsessing, hoarding, and neutralizing? This will be important for being able to identify the grouping of symptoms that a particular patient has. That is—in which categories do this patient’s symptoms fall?
There are many ways in which we can use the OCI-R
Above, we saw what the OCI-R consists of—18 symptoms belonging to 6 categories, with each symptom being rated from being “Not at all” to “Extremely” distressing or bothersome. Based on this, we can see that the OCI-R can be used for several different purposes:
1. To screen people for possible OCD
The OCI-R is the scale I recommend for this purpose. It has specifically been shown to be good for this purpose (Foa et al., 2002). If a person fills out the OCI-R and scores at or above a certain cut-off score (as explained below), the person probably has OCD.
Note: If a person screens positive on the OCI-R based on having a total score at or above the cut-off, this still does not mean that the person definitely has OCD. Only a clinical evaluation by a trained mental health professional can diagnose OCD.
Note: The OCI-R asks about current symptoms (in the last month). So, it does not screen people for past OCD.
2. To identify which OCD symptoms are present
Persons with OCD can have so many different symptoms. The OCI-R asks about 18 symptoms of OCD, so, with a quick glance at the OCI-R filled out by the person, we can see which symptoms are present.
3. To identify which groups of symptoms are present.
For example, one patient may have three of the 18 symptoms but all three may pertain to washing or cleanliness. Another patient may have four symptoms, two related to washing and two related to hoarding. The second patient has two different kinds of symptoms and may need two different kinds of interventions.
4. Evaluate the severity of the OCD symptoms that are present
As you see on the scale, for each symptom that is present, the scale also has the person rate how “distressed or bothered” they were by that symptom. This means that we see from the OCI-R which symptoms are most distressing or bothersome to the patient.
Scoring and interpretation
Each item on the Obsessive-Compulsive Inventory-Revised (OCI-R) can be scored on a 5 point scale from 0 to 4.
If we add up the scores on all the items, we get a total score, which can range from 0 (if the person rated all 18 items as 0) to 72 (if the person rated all 18 items as 4).
Try rating yourself on the OCI-R. When I did it, I found that I had some of these symptoms. Does that mean I probably have OCD?
The developers of the OCI-R recommended a cutoff score is 21. What this means is that persons whose total score on the OCI-R is 21 or more probably have OCD. Of course, the diagnosis has to be made or confirmed by clinical evaluation. (In case you are wondering, my score was less than 21.) This approach to using a cutoff score can be called “case finding”. That is, the scale is being used to try to identify patients who have OCD.
But, there is a huge problem with this approach. If a cutoff score of 21 is used, only 66% of patients with OCD will be identified (sensitivity) and the other one-third will be missed (false negatives; Foa et al., 2002). If we are using the OCI-R for screening, that is unacceptable.
Here is my own recommended solution to this problem:
As beautifully explained by Mark Zimmerman, MD, on another page on this website, when using an instrument for screening people, we must prioritize sensitivity and this can be done by lowering the cutoff score used. For the OCI-R, when a cutoff score of 5 was used, 99.5% of patients with OCD were identified (Foa et al., 2002). Of course, the downside (which cannot be avoided if the cutoff score is lowered) is that many persons who did not have OCD also had a score of 5 or more on the OCI-R. But, we are not going to use the OCI-R in isolation.
Here’s the key point—If the OCI-R suggests that a person MAY have OCD, we will carefully ask them several clinical questions. This is what we mean when we say that screening is done in two stages.
One more thing. Let’s use our common sense. Let’s suppose that a person rates just ONE symptom on the OCI-R as being present and “Extremely” distressing or bothersome. The total score will be 4. What are we going to say? That we are not going to evaluate this symptom because the total score on the OCI-R is less than 5? That would be ridiculous, right?
Bottom line: We should use the OCI-R for screening all patients who come to us for possible OCD at the initial evaluation. We should do ask clinical questions about possible OCD if either of the following is true:
– The person’s total score on the OCI-R is 5 or more
– The score on any one item is 2 or more
This will lead to a very high sensitivity. If neither of these is true, it is very unlikely that the person has OCD.
I hope you have started using the OCI-R in your patients already? I would love to hear about your experiences with this scale. Please post your comments at the bottom of this page (under “Leave a Reply”).
Related Pages
Self-rating scales for OCD: Why? How? Which ones?
References
Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, Salkovskis PM. The Obsessive-Compulsive Inventory: development and validation of a short version. Psychol Assess. 2002 Dec;14(4):485-96. PubMed PMID: 12501574.
Huppert JD, Walther MR, Hajcak G, Yadin E, Foa EB, Simpson HB, Liebowitz MR. The OCI-R: validation of the subscales in a clinical sample. J Anxiety Disord. 2007;21(3):394-406. Epub 2006 Jun 30. PubMed PMID: 16814981.
Copyright © 2020 to 2025, Simple and Practical Medical Education, LLC. All rights reserved. The content on this website may not be reproduced in any form without express written permission.
Disclaimer: The content on this website is provided as general education for medical professionals. It is not intended or recommended for patients or other laypersons or as a substitute for medical advice, diagnosis, or treatment. Patients must always consult a qualified health care professional regarding their diagnosis and treatment. Healthcare professionals should always check this website for the most recently updated information.